 |
By Jacqueline Carrico, BS, MD
Despite very promising results of CAR-T therapy in acute lymphoblastic leukemia, B-ALL, antigen-loss relapse has arisen as a major challenge for maintaining long term remission. Here we will review the potential mechanisms for antigen-loss relapse and some novel strategies to combat this problem.
One possible mechanism for antigen loss is downregulation of expression of the target protein in the malignant cells. Constant therapeutic stress from the highly-targeted CAR T-cells may lead to this phenomenon. Additionally, tumor cells may express an alternative form of the receptor via mutation or alternative splicing. In this case, the receptor may take on a form which is no longer recognizable by the chimeric antigen-receptor.
It has been hypothesized that distributing the therapeutic stress to two tumor markers may prolong the duration of remission. Two novel approaches have been developed: dual-signaling CAR-T and tandem CAR-T. Dual signaling CAR-T cells are two distinct CAR molecules with distinct binding domains, targeted at two unique tumor proteins. Meanwhile, tandem CAR-T cells have one CAR molecule expressing two distinct binding domains in tandem. In B-ALL, CD19 has been involved in antigen escape after anti-CD19 CAR-T therapy. Thus, the development of CAR-T cells targeting other pan-B cell markers, such as CD20 and CD22, are thought to be ideal targets for dual or tandem CAR-T therapy. A major concern with dual or tandem CAR-T is the possibility of cytokine release syndrome, given a significant increase in antitumor activity seen with these techniques. It is still unknown if this dual selective pressure could cause antigen loss of both targets simultaneously.
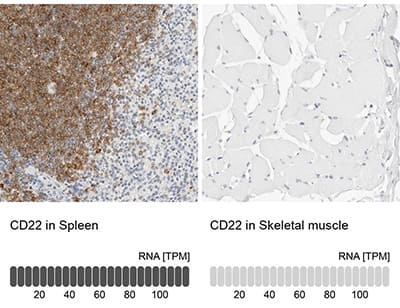 Immunohistochemistry-Paraffin: Siglec-2/CD22 Antibody [NBP1-87041] - Staining in human spleen and skeletal muscle tissues using anti-CD22 antibody. Corresponding CD22 RNA-seq data are presented for the same tissues.
Immunohistochemistry-Paraffin: Siglec-2/CD22 Antibody [NBP1-87041] - Staining in human spleen and skeletal muscle tissues using anti-CD22 antibody. Corresponding CD22 RNA-seq data are presented for the same tissues.
A challenge in developing these therapies is the difficulty in finding specific targets that will allow antitumor activity without significant on-target/off-tumor toxicities. An ideal target for CAR-T therapy is one that is highly expressed in tumor cells, participates in malignant progression, and is expressed in low amounts in healthy tissues. One ideal example is EGFRvIII, a variant of the epidermal growth factor receptor which is found only in malignant cells. Preliminary studies targeting EGFRvIII have shown promising results, though the potential for antigen escape still exists. Unfortunately, this is the only target that has been identified in solid tumors with no expression in healthy tissues.
Many more studies will be necessary to understand the efficacy and safety of these novel approaches. In theory, targeting additional antigens seems like a logical and promising way to achieve prolonged remission. The biggest challenge will be the identification of novel targets that are both efficacious and safe, as on-target/off-tumor toxicities have already been a limitation in CAR-T therapy.
 Jacqueline Carrico, MD
Jacqueline Carrico, MD
University of Colorado, School of Medicine
Jackie is completing her medical training in Anesthesiology and has a diverse background in basic science, translational, and clinical research.
References
Wang Z, Wu Z, Liu Y, Han W. New development in CAR-T cell therapy. J Hematol Oncol. 2017;10(1):53.